Bacterial vaginosis during the menopause
Does this sound familiar? There is a fishy smell, a thin, milky discharge is coming out of the vagina and you experience a burning sensation when urinating or having sex.
Bacterial vaginosis during the menopause: Signs and symptoms
Does this sound familiar? There is a fishy smell, a thin, milky discharge is coming out of the vagina and you experience a burning sensation when urinating or having sex. These are typical signs of bacterial vaginosis. Read more in this article to find out what bacterial vaginosis is, how it manifests, what facilitates it and what you can do about it.

Vaginal infections and vaginitis are some of the most common gynaecological illnesses and can occur in women of all ages. Almost every woman experiences them, and they often occur in sexually active and pregnant women. The oestrogen deficiency during the menopause also facilitates these complaints. Bacterial vaginosis is the most common bacterial vaginitis found in women of reproductive age and is triggered by bacteria, as the name already suggests. This is usually the species Gardnerella vaginalis, which causes the characteristic fishy smell (med. amine smell).
If the vaginal balance is disrupted and the natural acid resistance in the vagina is no longer able to keep undesirable pathogens in check, pathogenic germs can prevail in the vagina. To be precise, bacterial vaginosis is not an infection and is therefore referred to medically as dysbiosis (imbalance). It is also not a sexually transmitted disease.
Typical indications of bacterial vaginosis are an increase in grey-white to yellow, thin discharge and usually a fishy, sometimes even sweetish smell around the vagina. Almost all cases of bacterial vaginosis show an elevated vaginal pH value of over 4.5, while this remains in the normal acidic range with thrush.
Inflammation of the vagina is rare in bacterial vaginosis (unlike with thrush), but itching, burning and skin irritation around the outer vaginal area can occur, as well as pain when urinating or having sex.
Not all of these indications have to appear together and around half of women affected do not even notice the infection, as in these cases, bacterial vaginosis is extensively symptom-free. Risk factors are, in particular, unprotected sex as well as stress, smoking, excessive or incorrect vaginal hygiene and hormonal changes during pregnancy or the menopause.

Bacterial vaginosis or thrush? How to tell the difference.
|
|
|
|
|---|---|---|
|
Vaginal discharge |
Increase in grey-white to yellow, thin discharge |
Whitish, thick, partially crumbly discharge |
|
Vagina smell |
Typically fishy, sometimes even sweet |
Unspecific |
|
Complaints |
Sometimes burning when urinating or having sex |
Typically vaginitis with swelling and reddening of the vaginal mucosa with white coatings, accompanied by itching and burning. |
Bacterial vaginosis during the menopause – What you need to know
Bacterial vaginosis mainly occurs in sexually active women with unprotected sexual intercourse. With a pH value of 7.2–7.8, the male sperm is alkaline (basic) and thus weakens the natural acid resistance of the vagina by increasing the pH value of the vagina short term. The vagina is not always able to break down or compensate for this pH value increase again quickly and this can result in a longer-term or lasting imbalance in the vaginal flora. However, even women going through hormonal changes such as during pregnancy, after giving birth or during the menopause can experience bacterial vaginosis frequently.
Slightly more than half of all women experience bacterial vaginosis at least once in their lifetime.
Almost one in three cases of bacterial vaginosis heals spontaneously.
The recurrence rate is relatively high at 60–70%.
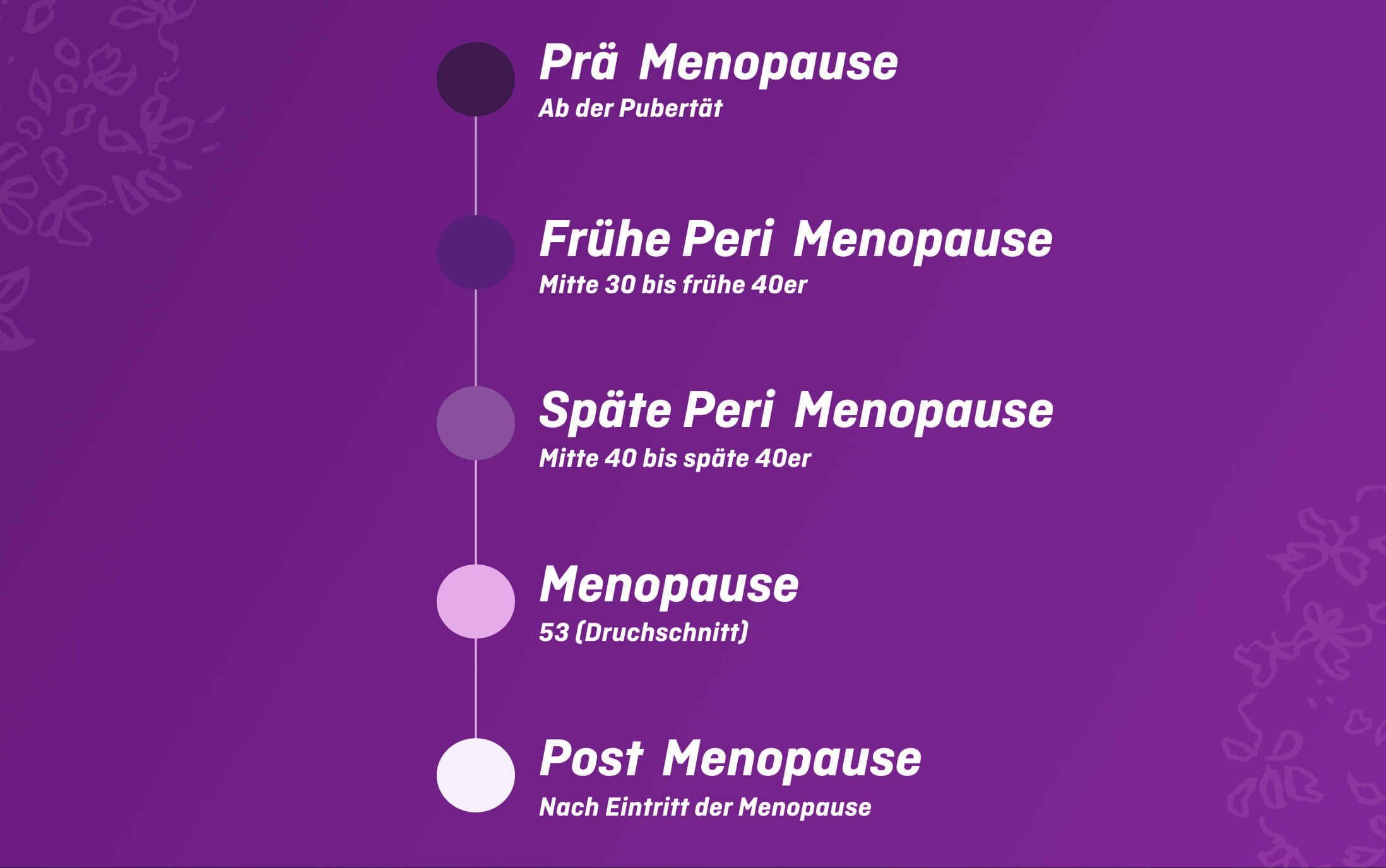
Hormonal changes in the menopause can cause the pH value in the vaginal environment to increase and the natural acid resistance to weaken, enabling pathogenic germs in the vagina to prevail more easily and increase susceptibility for vaginitis.
A further consequence of the falling oestrogen level during the menopause is that the vaginal mucosa (known as vaginal atrophy) becomes thinner. This goes hand in hand with increased susceptibility to vaginal inflammations and infections. Atrophic vaginitis (also known as atrophic colpitis) occurs particularly during the postmenopause or in women who have already had their oestrogen production inhibited through medication or operations, such as during cancer treatment.

Bacterial vaginosis during the menopause: Prevention and treatment
There are several things you can do to prevent vaginitis. But first, it is important to understand the vaginal balance.
A healthy vagina has a natural balance, which is maintained by the natural acid resistance and natural vaginal moisture and can sometimes be disrupted by different influences.
The healthy vagina usually has a high amount of lactic acid bacteria in its microbiota. Known as lactobacilli, they produce lactic acid and some types also produce hydrogen peroxide (H2O2). This healthy, acidic and antibacterial environment keeps pathogens at bay and protects the vagina from infection in a very natural way. The lactic acid bacteria also rely on the natural moisture of the vagina to fulfil their important task. For this reason, women who suffer from vaginal dryness are more susceptible to vaginal infections.
The vaginal balance can be supported by a suitable diet (such as probiotics or refraining from excessive carbohydrate consumption) and sufficient liquid intake with healthy drinks such as water or tea and, if any risk factors are present or there is a tendency towards vaginitis, strengthened or restored using acidifying remedies.
Moisture in the vagina
If you frequently suffer from bacterial vaginosis or have a predisposition to do so, it may be sensible to make a preventive treatment with acidifying remedies to support the natural acid resistance and restoration of the vaginal balance.
For menopausal women with accompanying vaginal dryness as a possible cause, it is advised to combine these with moisturising remedies.
There are some tips you should know if you have a tendency towards vaginitis:
Avoid unprotected sex: Disruptions to the vaginal environment are mainly widespread in sexually active women. Sperm weakens the vaginal acid resistance. For this reason, you should avoid unprotected sex, especially if you are at higher risk of vaginitis.
Check your vaginal hygiene: Excessive vaginal hygiene with cleansers or sprays that are too strong can disrupt the natural balance. Mild cleansing lotions especially tailored to the vagina and containing natural ingredients, gentle drying and looser, pure cotton underwear are better. Likewise, make sure to only wipe from front to back after going to the toilet to prevent any germs from entering the vagina.
Relieve vaginal dryness: Vaginal dryness, e.g. in the menopause can also facilitate susceptibility to vaginal infections, as the lactic acid bacteria prefer a moist environment.
Drink enough: Make sure to get enough fluids with healthy drinks such as water or unsweetened tea. This will also do your skin good.
Reduce or give up smoking: If you smoke, you should think about restricting your consumption or best of all, stop completely, as smoking influences the vaginal balance long term.
menoelle® and bacterial vaginosis
menoelle® OVULA med is a medical product that helps maintain the natural defences of the vagina and promotes the restoration of healthy vaginal flora.
Lactic acid, normally present in the vagina, favours an immediate pH correction and facilitates the natural recovery of the delicate vulvo-vaginal ecosystem. Boric acid, thanks to its persistence in the vaginal environment, favours a lowering of pH prolonged over time.
Hyaluronic acid exerts a hydrating and lubricating action against vaginal dryness and helps to restore a natural and comfortable vaginal environment.
A treatment with menoelle® OVULA med Vaginal Suppositories can restore and preserve vaginal health.
Cue: Visit the doctor
In the case of acute bacterial vaginosis, you should visit your gynaecologist, as this can lead to increased infections and the recurrence rate of 60–70% is relatively high. After an examination, the diagnosis can be made and a targeted therapy initiated with an effective means for localised use in the vagina. Even if this disease might be unpleasant for you, there is no room for shame here.
Bacterial vaginosis can significantly increase the risk of rising gynaecological infections, such as at the cervix, the fallopian tubes or the ovaries. Numerous study results also suggest that untreated bacterial vaginosis can lead more often to premature births. Purely acidifying medication (or other household remedies) are usually not suitable for fighting acute vaginitis.

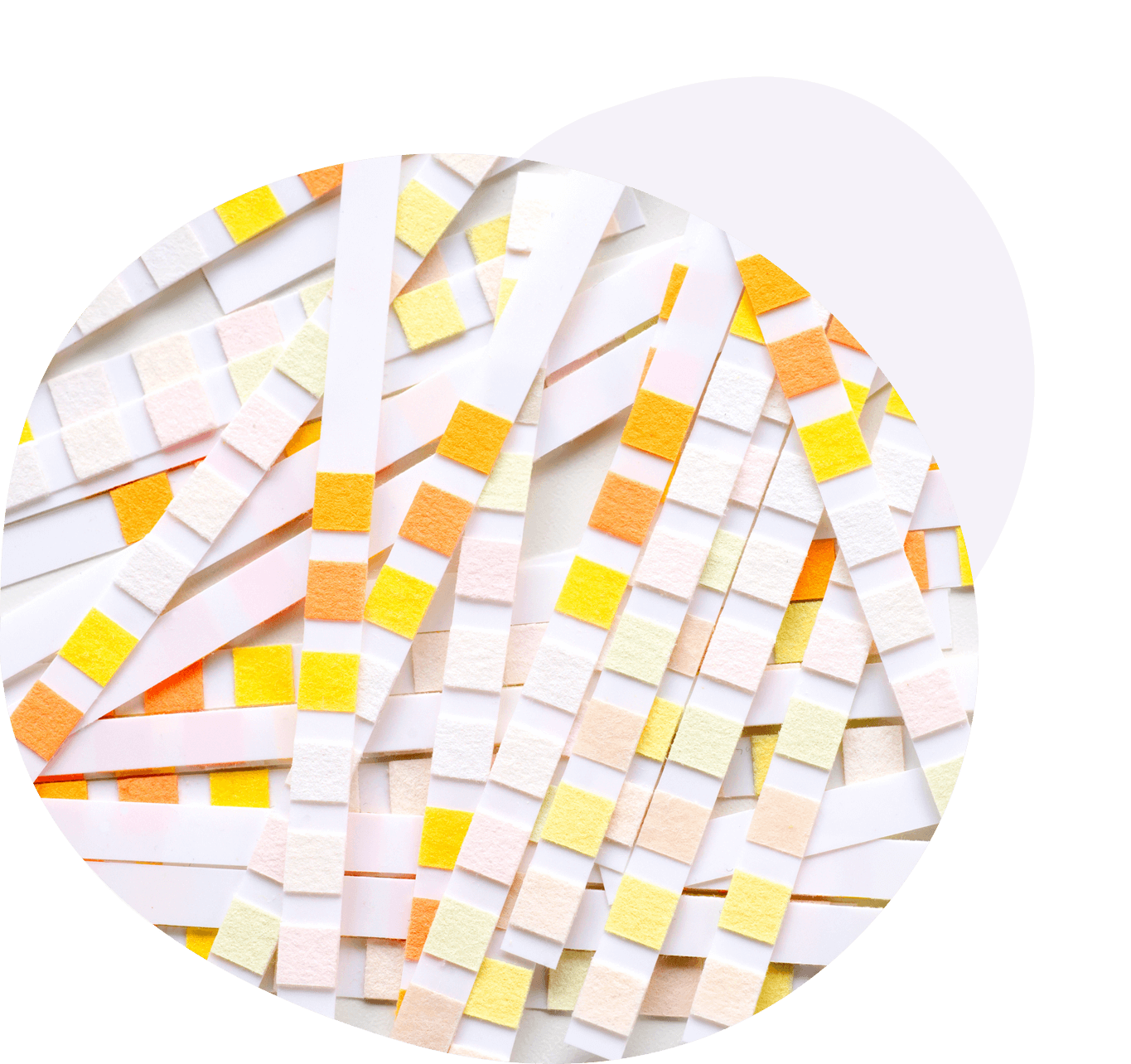
Check your pH value yourself
A simple test that you can perform yourself quickly provides information about your vaginal pH value and helps to detect bacterial vaginosis early on and treat it in good time. For this, special test sets are usually available from pharmacies or chemists’ and allow you to easily check your vaginal pH value at home.
While the versions are different, the principle is always similar. Take some vaginal secretion using a test stick and compare the test result with the enclosed colour scale. With an elevated pH value – especially with values of over 4.5 – you should increase your awareness about the topic of vaginitis.